Registered Psychologist with Trauma Services at Royal Inland Hospital
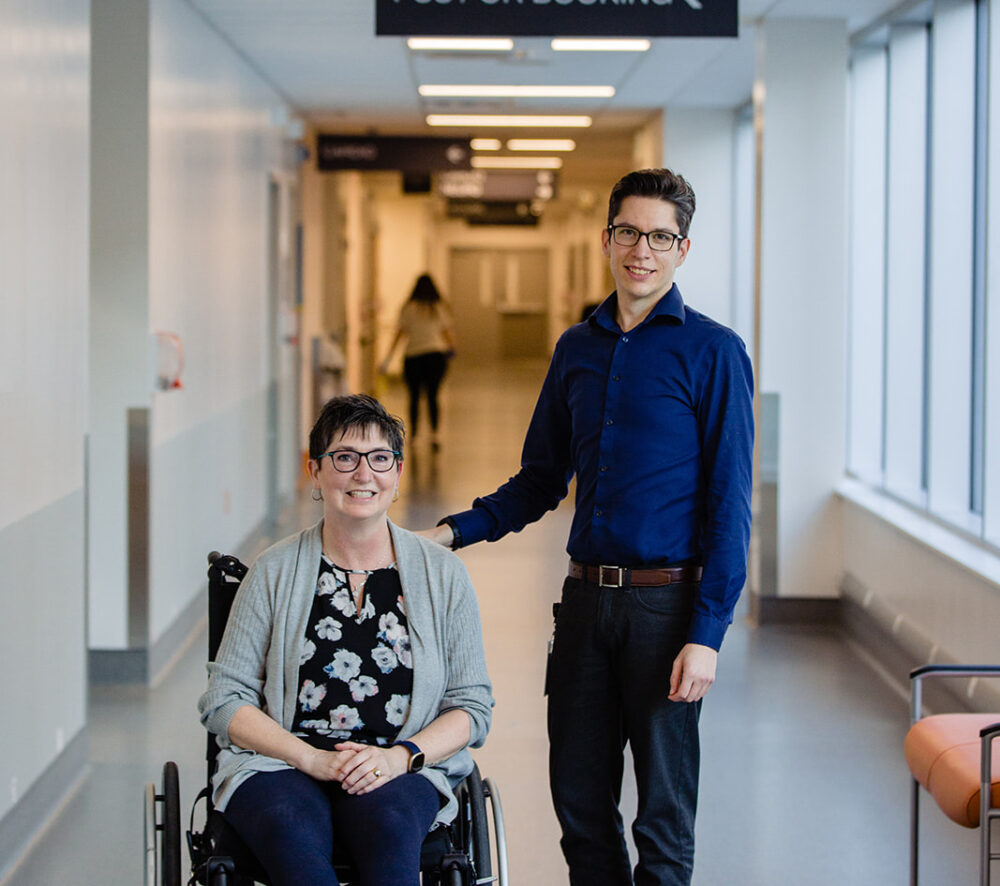
Meet Dr. Logan Nealis, Royal Inland Hospital’s very own Registered Psychologist and learn about the invaluable role he plays working with the RIH’s Trauma Services.
His work is nothing short of remarkable. Each and everyday, he touches the lives of patients in a profound way. As one of his past patients recovering from a horrible motor vehicle accident explains, “When things got tough, Logan reignited my drive to keep moving forward. I wouldn’t be where I am today without him. He completely changed my mindset and as a result, I have had far more good days than bad.”
In this spotlight, you will bear witness to the passion and dedication Dr. Nealis carries with his profession and learn about his essential role in taking a holistic approach to caring for patients and their families.
Can you provide a brief description of your background?
I often describe myself as a nomad at heart – I grew up in the Central Interior of BC and gradually migrated east over the course of my education. My interest in psychology stems from a desire to understand what goes on “under the hood” of our human experience – from our mundane everyday life to pathological syndromes. It felt like a natural progression to pursue this as a career. I obtained my doctorate in Clinical Psychology from Dalhousie University in Halifax, and then I made my way back west to complete my clinical residency in Edmonton. For the past three years, I worked with the Cross Cancer Institute in Edmonton where I provided psychological care to people affected by cancer. That experience highlighted the importance of being close to family, so my partner and I decided to return to BC. The transition from working with critical illness to critical injury also felt like a natural next step, so I joined the Trauma Services team at RIH.
Can you describe a day in the life of a registered psychologist working with trauma services?
The excitement, and challenge, of working in acute care is that every day is unique. I always meet with the rest of the trauma team to review current admissions and discuss anyone who might benefit from psychology before making a plan for the day. Sometimes, the priority is in working directly with a patient or their family to support psychological needs that arise. Other times, I might meet with other members of the multidisciplinary team to discuss a patient’s care or how to support them after discharge. Whenever possible, I also make time to get involved in educational opportunities for staff (e.g., nurses, allied health) to talk about how to better identify and support the emotional needs of patients and families. It is a very diverse role.
Can you describe the Trauma Services Program at RIH and the team you work with?
The Trauma Services Program at RIH is part of a regional network in Interior Health that views traumatic injury from an integrated systems-based perspective. With the right expertise and processes in place, secondary injuries or medical complications can be identified and addressed efficiently to improve quality of care for patients, shorten hospital stays, and reduce risk of complications post-discharge. Psychological injury and emotional adjustment is considered as part of that broad perspective. The trauma team here at RIH includes a group of general surgeons who complete weekly rotations on the service, the Trauma Nurse Coordinator (Brad Stroich), a data analyst, and me as the psychologist. We are incredibly lucky to have a dedicated team of nursing staff and allied health professionals on the Neuroscience and Trauma Unit (8th Floor, Phil & Jennie Gaglardi Tower) that support our patients directly in their day-to-day care. We also have a fantastic regional director and other team members in Kelowna who support our work in important ways.
What formal training/education do you need to become a registered psychologist? Do you need special training to work with trauma patients in particular?
Psychology is a regulated health profession, so we have strict criteria we need to meet to be eligible for registration. Generally speaking, that involves a doctoral degree (e.g., Ph.D. or Psy.D.) in clinical psychology, completion of an accredited residency program, and completion of licensing exams. Assessment and early intervention for psychological trauma is an important part of my role with Trauma Services, so specialized training and experience in this area is critical. There is also an area of specialized training known as health psychology, which is all about how to apply psychological principles to the maintenance of health and adjustment to health-related difficulties. Although this is not strictly required to work with trauma patients, it helps to better understand the role of psychology in the healthcare system and be more effective in this role.
In a simple “elevator pitch” can you describe your role in healthcare?
In a healthcare crisis, normal every-day people find themselves in unfamiliar and overwhelming circumstances. My role is to help people navigate these challenges so they can continue living a meaningful life, regardless of the circumstances they’re facing.
What impact do you hope to make with your work?
My hope is to highlight that psychological health is just as important as our physical health – and in some cases, the two go hand-in-hand. Even if the people I work with only come away with one or two new insights, small changes can have a significant long-term impact.
What is the most rewarding part of your profession?
I am a firm believer that our thoughts, emotions, and behaviors can be understood so that our daily experiences feel less confusing and overwhelming. There are ways of becoming unstuck if we have the right road maps and a supportive guide. The most rewarding part of clinical practice is when I get to see a new idea “click” for someone, and suddenly a challenge that felt insurmountable begins to feel less formidable to them.
What set of values do you try to live by everyday?
Curiosity, flexibility, and humility are my most important guiding principles, both personally and professionally.
What is your favorite part about living and working in Kamloops?
I really appreciate the down-to-earth feel of Kamloops –there’s a real sense of authenticity to it. As a self-described nature nerd, Kamloops is also a very convenient place to be. We have access to everything from coastal rainforest to grasslands to alpine meadows all within a four-hour drive. Having lived in numerous places from coast to coast, the interior is really unique in that way. Opportunities for outdoor recreation are essentially limitless.
What does the future hold for you?
In addition to my clinical role, I have also taken on the role of Professional Practice Lead for psychology in the Thompson-Cariboo region. With this additional role, I anticipate keeping myself busy for the foreseeable future as we continue to advocate for, and develop, the role of psychology in the region.

